Case study – Dementia reducing stress and distress at Royal Infirmary Edinburgh: September 2025
Improving early identification and support of stress and distress in an Acute Medicine of the Elderly ward at the Royal Infirmary Edinburgh.
Introduction
Staff in ward 202 at the Royal Infirmary Edinburgh recognised a rise in stress and distress behaviour in patients on the ward, leading to an increase in the length of time spent in hospital. The team joined the Reducing Stress and Distress Improvement Programme and were able to identify and implement improvement ideas to enhance identification and person-centred care for patients living with dementia.
Situation
Ward 202 is a 36-bedded, Acute Medicine of the Elderly ward in the Royal Infirmary Edinburgh. Staff had identified an increase in numbers of patients on the ward with high levels of stress and distress. This was resulting in longer hospital stays. The team recognised a need to improve how they identify and provide appropriate care for these patients and signed up to the Reducing Stress and Distress Improvement Programme. The team involved in the programme included the Senior Charge Nurse, Clinical Practice Facilitator, Stress and Distress Lead Nurse, and Occupational Therapy Team Lead with support from NHS Lothian Dementia Consultant.
By working through the Reducing Stress and Distress Self-Evaluation Tool the team identified several key opportunities for improvement.
- Introduce formal process and tools to identify and assess stress and distressed behaviours in patients living with dementia and/or delirium.
- Increase use of stress and distress care plan to ensure quality, person-centred care is being provided.
- Build capacity and confidence in staff to identify and support patients at risk or experiencing stress and distress.
Royal Infirmary Edinburgh
Approach
Non-urgent advice: Aim
Following completion of the Self-Evaluation Tool, the team conducted a wider staff consultation to better understand their current system. The team were supported by their coach at Healthcare Improvement Scotland to carry out a process mapping exercise. This highlighted how staff currently identified and supported patients with stress and distress from admission through to discharge. Gaps and opportunities for improvement were then identified. A key issue across all staff groups was variance in understanding of the definition of stress and distress and confidence in using appropriate person-centred approaches to support behaviour. Staff also identified challenges in communication with lack of a robust process for information sharing and review within the multidisciplinary team (MDT). This led to missed opportunities to intervene earlier to prevent distress with staff tending to respond reactively to distressed behaviour.
Several change ideas were then developed and tested on the ward to address these challenges. This included:
- implementing a flowchart to create a clear process across the MDT to identify and support patients with stress and distress
- using a Stress and Distress Care Plan to plan and deliver person-centred care to support patients with stress and distress
- staff training on definition of stress and distress and completion of Stress and Distress Care Plans
The flowchart included several changes to processes within the ward. Staff training was completed to raise awareness of these new processes and ensure they were implemented consistently:
- Use 4AT (delirium detection tool) and patient history to identify patients at risk of experiencing stress and distress
- Patients identified discussed daily by the MDT at the ward safety brief. Magnets used to identify patients on the patient board in the ward base
- ‘Getting To Know Me’ (GTKM) form completed with unpaid carers/family members. GTKM is a person-centred care resource used in hospitals for patients with dementia or cognitive impairment. It helps staff understand the individual behind the patient and aims to enhance communication, dignity, and person-centred care.
- GTKM information used to inform a stress and distress care plan that included person-centred support strategies for each patient.
To monitor compliance and impact of these processes the Stress and Distress Lead Nurse completed weekly audits to look at whether strategies identified in the stress and distress care plan were reflected in the care provided.
Results
The team identified an increased number of patients with dementia or at risk of experiencing stress and distress through implementing their change ideas. They also saw an increase in the number of Stress and Distress Care Plans completed. The team is currently investigating if this is being done within 72 hours of admission. There has been a sustained change in practice as stress and distress is now a standing item on the daily safety brief agenda. This ensures the MDT will continue to identify and discuss patients daily who are at risk or are experiencing stress and distress.
Ward 202 has reported notable improvement in compliance with the Lothian Accreditation and Care Assurance Standards (LACAS). From December 2024 to July 2025, Standard 11 (care of vulnerable adults) increased by 32%, from 50% to 82%, while Standard 11b (care of patients with altered cognition) rose by 31%, from 33% to 64%. These improvements are attributed to the ongoing improvement work being undertaken by the team.
Table 1: Percentage of patients with known dementia or cognitive impairment who have GTKM completed in ward 202 Royal Infirmary Edinburgh
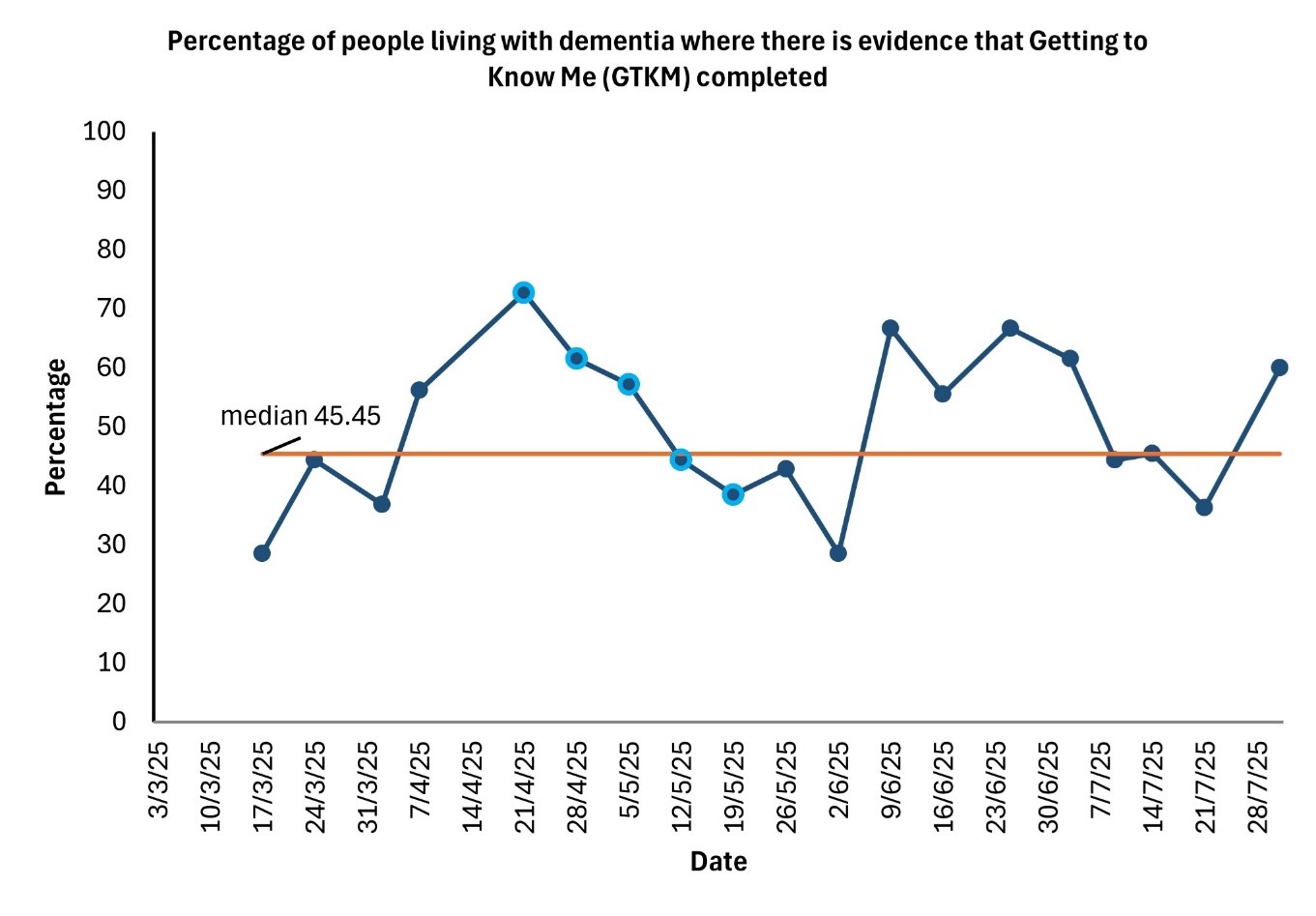
The table shows a general increase in number of GTKM completed for patients living with dementia with a median of 45% completion. Staff have reported challenges in completing GTKM as often family members or carers are not present during the patient’s hospital stay.
Table 2: Percentage of patients identified at safety brief who have a Stress and Distress Care Plan completed in Ward 202 Royal Infirmary Edinburgh
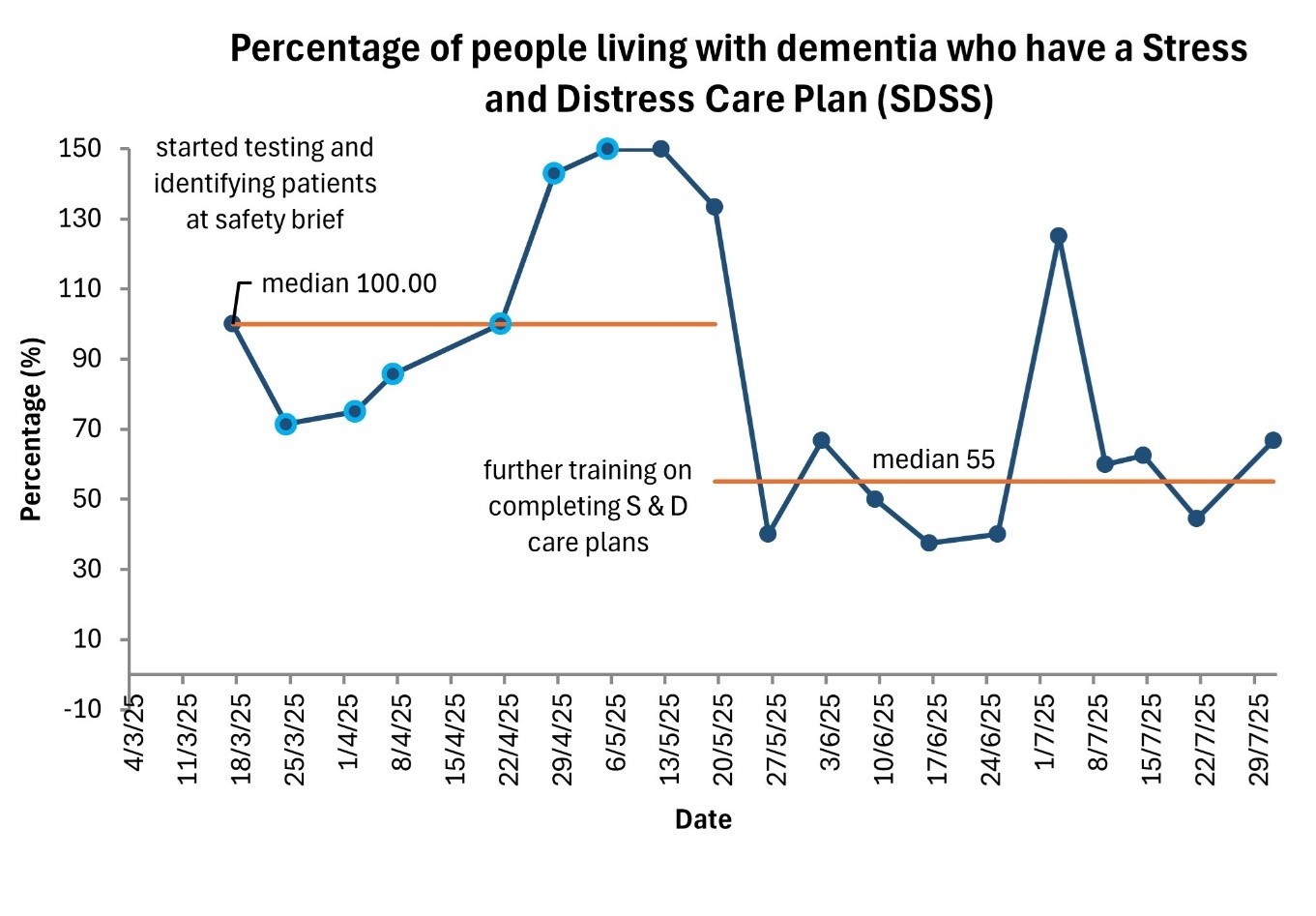
This table demonstrates how successfully the Stress and Distress Care Plan has been implemented. Following initial staff training, these plans were introduced on 18 March 2025. At first staff were over enthusiastic in their approach and completed more care plans than patients who had been identified. By capturing this data, the Stress and Distress Lead Nurse was able to refine the training and improve staff understanding of why and when a Stress and Distress Care Plan should be completed. Following further training the number of plans dropped and is now at a median of 55%.
Staff feedback has highlighted improved understanding of the definition of stress and distress and in recognising which patients should be identified at the safety brief. Staff are more confident that patients are identified and supported earlier.
“It is helpful to put theory into practice and think about developing interventions.”
Royal Infirmary Edinburgh

I observed many nurses with very patient approaches and lovely attitudes to the patients with very high behavioural / distress care needs
Royal Infirmary Edinburgh
Key learning
Top tips:
- Try not to be overly critical during the self-evaluation process. When scoring the Self-Evaluation Tool, aim for honesty without harshness. Being too critical can cloud the team’s judgment and undermine the team’s confidence. Instead, maintain a balanced perspective— acknowledge the team’s successes and strengths alongside the challenges faced. This mindset helps the team to stay motivated and make meaningful progress.
- Work smarter using a team-based approach. Instead of one person trying to do everything, divide tasks across the team based on strengths and capacity. This not only lightens the load but also brings diverse perspectives to the table. A well-co-ordinated team with clear communication and agreed roles and responsibilities is far more likely to deliver sustainable results.

The introduction of change ideas aligned to existing processes has enabled a sustained shift in practice. Identifying patients at risk of stress and distress behaviour is now standard ward practice as is a standing agenda item in the safety brief and has ensured that all staff are involved. The weekly audit has enabled ongoing monitoring of implementation, highlighted further opportunities for further staff development and has supported sustainability.
Having data to demonstrate impact was essential to gain buy-in from the wider team. Initial resistance was overcome by demonstrating evidence of the impact on patient care. It was helpful to have team members with quality improvement knowledge and to be able to access NHS Lothian’s Quality Improvement Team for support with data collection.
Being part of an improvement programme and working alongside other hospitals and care homes was very supportive and encouraged learning. The Self-Evaluation Tool was helpful to identify improvement priorities and to focus on activity as a team. At times, the team was frustrated with lack of progress but hearing from other teams and recognising shared challenges kept the motivation to continue. The team connected with another NHS Lothian team in the cohort and were able to find a solution to logging GTKM information in the electronic patient records.
“Staff had documented non-pharmacological strategies throughout the patient’s admission, this provided more evidence towards diagnosis”
Royal Infirmary Edinburgh
Next steps
The team will continue to raise awareness of the flowchart with the aim of embedding this as a way of working on the ward. The Stress and Distress Lead Nurse will continue with weekly audits of the Stress and Distress Care Plans with a focus on improving the quality of these through ongoing staff training. Data will continue to be collected to evidence the impact of this and on the care patients receive. The Stress and Distress Symptom Scale is being tested as a mechanism to evaluate if person centred strategies are having an impact on patient experience.
The team are now looking at the next priorities identified through the self-evaluation tool. This includes the following.
- Reviewing the flowchart to expand more on the process for patients with delirium to include sudden or gradual onset.
- Working with staff to increase the number of GTKM and Stress and Distress Care Plans completed for patients within 72 hours of admission.
- Increasing the involvement of volunteers, working with families and carers, to support meaningful activities in the ward. This includes capturing information on the impact of meaningful activity for patients living with dementia.
- Developing simulation training on the clinical skill of de-escalation that will be open to the whole multidisciplinary team. The team are in contact with other teams participating in the Reducing Stress and Distress Improvement Programme to learn from their activity.
